Article updated May 2023.
What is patient insight, and why is it critical to pharmaceutical teams?
Prioritizing patients during clinical trial design and execution is proven to increase trial success – in a study comparing trials with significant patient-centered elements to traditional trials, 87% of the patient-centered trials had positive results, much higher than 68% for the traditional trials. And companies that take more patient-centric approaches to trial design and execution have moved the needle on reducing average trial enrollment time and shortening the timeline from first patient dose to product launch.
But according to the NIH, approximately 85% of patients were unaware that clinical trials existed, let alone that they could participate in them. Of those, 75% of the patients said they would have been willing to enroll in a trial had they known about it. Getting more patients involved in trials from the early stages can provide trial sponsors with more data that might change how effectively trials are conducted and how quickly new treatments can begin improving patients’ lives.
What is patient insight?
Patient insights give healthcare providers and life science companies the capacity to accurately understand the experience of having a specific health condition. By gaining an in-depth understanding of the patient experience – listening to patient needs and gathering evidence about what is influencing their healthcare journey – health organizations can improve outcomes for other patients.
In listening to patients, life science companies can capture any unique experience, patient perspective, needs, and priorities. Some examples include:
- Symptoms of different conditions
- Impact of the condition on patient quality of life
- Experience with previous treatments
- Outcomes that are important to patients
By transforming patient insights into relevant actions, trial sponsors can create patient-centric trials that produce more successful outcomes. Patient insights can also help a healthcare organization create a more patient-centric culture or deepen its commitment to patient-centric drug development.
Why is patient insight important?
Patient insight comes directly from people with the most relevant experience – their health. HCPs know the science but typically don’t have first-hand experience with the disease or condition they treat. Patient data in healthcare and insight are the closest they can get to a more complete understanding of what it’s like to be diagnosed or treated for a health condition.
In clinical trial design, a patient-centric approach can involve patients at almost any point. Patients can provide:
- Input on trial design elements such as site locations and clinic visit frequency
- Feedback on proposed patient-facing resources, such as educational materials or clinical trial enrollment websites
- Information on the condition that is being studied and how it affects day-to-day life
By building trials that specifically consider patients’ experiences, trial sponsors are more likely to see fewer participants who choose to discontinue the trial, more patient diversity in enrollment, and more insightful patient feedback overall.
Patients are a key part of the scientific narrative that develops over a product’s lifecycle. While physicians can share what their patients tell them, patients can directly share their lived experiences. This provides an outlet for patients and supplies life science companies with valuable insights that help shape product and drug development. These insights – paired with that of physicians and other healthcare professionals – create a more complete picture of specific disease communities.
What is patient data in healthcare?
Patient data is medical information about an individual patient, including information about their past and current health or illness, treatment history, and genetic data. It can also include biometric data or measurable physical characteristics that a machine or computer can check. This type of clinical data might be created or received by a healthcare provider, payer, employer, or other person involved in providing care to an individual. Patient data fall into six general categories:
- Electronic health records. Electronic health data is obtained at the point of care, such as a medical facility, hospital, or clinic. An electronic medical record or EMR might contain information about demographics, diagnosis, treatment, prescription drugs, lab tests, hospitalizations, and insurance.
- Administrative data. This data includes hospital discharge information that might be reported to government agencies or other entities.
- Claims data. Claims data includes the billable interactions between insured patients and a healthcare provider and falls into four main types: inpatient, outpatient, pharmacy, and enrollment.
- Patient/disease registries. Disease registries are clinical information systems that track key data for chronic conditions like cancer, diabetes, heart disease, and asthma. These resources can provide critical information for managing patient conditions.
- Health surveys. National health surveys of chronic conditions can evaluate population health and disease prevalence estimates. These data sources are compiled specifically for clinical research purposes and are widely accessible.
- Clinical trials data. These registries offer varying degrees of access to data.
How can pharma companies achieve better patient engagement?
Medical device and pharma companies work hard to understand patient needs but sometimes hesitate to expand patient engagement strategies. Traditional barriers to better patient engagement center around compliance, patient privacy, and logistics:
- Pharma and medical device companies may be reluctant to engage patients to avoid risk
- Patients may find it difficult to share sensitive medical information in face-to-face meetings
- Patients dealing with conditions that cause them to feel unwell or make it difficult to travel may decline to participate in engagements that are inconvenient
- Video meetings may be unmanageable for both experts and patients due to work or family commitments
However, life science teams have found a way to be compliant while still prioritizing patient engagement by using a virtual engagement platform, which takes place over a period of days or weeks and allows participants to answer questions on their own schedule. These capabilities became even more important during the COVID-19 pandemic, when clinical trials, patient advisory boards, and other patient-facing activities needed to continue amid lockdowns and travel restrictions. Now, pharmaceutical and medical device teams prioritize virtual engagement as part of a more holistic insights management strategy. This approach treats insight-gathering as a single strategic process rather than a disconnected series of siloed activities.
This is a time of high positive sentiment for life science companies in patients’ minds. Before the pandemic, just 47% of patients said they felt pharmaceutical companies understood their emotional, financial, and other needs related to their condition, and only a third reported interacting with a pharmaceutical company regularly. But new research shows that patient trust in the healthcare ecosystem has increased overall, with a boost of 45% for pharmaceutical companies and 44% for medical device companies.
How do you encourage patient engagement?
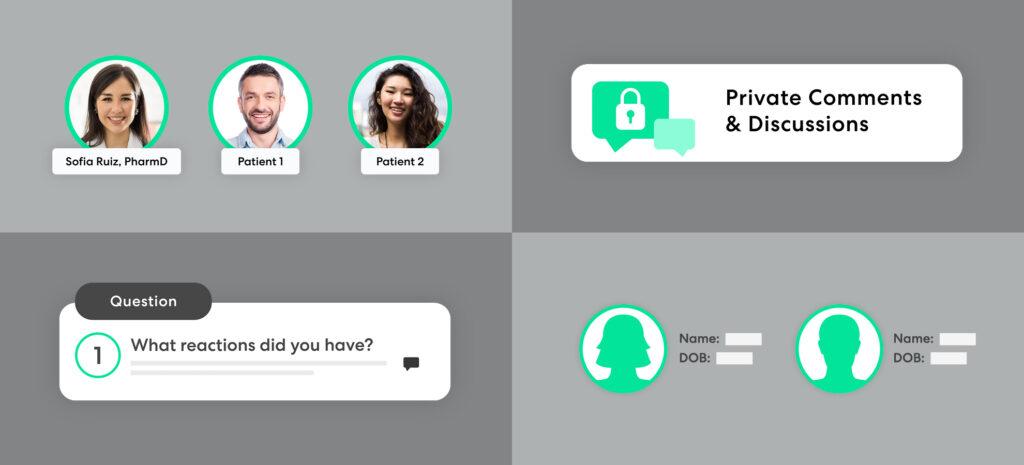
Designing effective patient engagements requires a few key elements that will ensure success and keep patients feeling comfortable about their participation. These key elements include:
- Choosing the right participants – both patients and moderators
- Conducting blind or double-blind sessions when appropriate
- Choosing the right questions to prompt robust discussion
- Maintaining confidentiality
- Choosing the right participants
Teams need to be certain they are engaging with the right patients for participation – those who meet specific criteria and are able to participate within the time frame for the virtual meeting. Communicate clearly to patients about what to expect during the online session, including what your team is hoping to achieve. Recognize that there might be varying levels of digital-savvy among patients, and offer how-to or welcome documentation accordingly.
Blind and double-blind sessions
Protecting the identity of patients during a session can be necessary to ensure compliance. Pharmaceutical teams can offer anonymity by creating a naming convention, such as initials or generic names. Names and logos of pharmaceutical companies can also be hidden by using an unbranded online space when desired. If there is a webcast component to the session, we recommend using a webinar option that does not enable members to see one another.
Questions and content
Asking the right questions will help pharmaceutical teams get the insight they need to achieve their objectives. Varying the types of questions asked will also help keep the participants’ interest during a session, particularly if there are many questions. Be mindful that discussing personal details about a challenging medical condition can be difficult for some patients. If necessary, teams can also include language that provides patients additional resources or help, such as crisis hotlines or other ways to contact experts for assistance.
Maintaining confidentiality
Life science teams can take advantage of several opportunities to remind participants of the need for confidentiality. Orientation training or any contact before the meeting is a good time to do this. For the most part, simply reminding participants not to include any identifying information, names, or other personally identifiable information should suffice.
Looking for more information on conducting successful patient engagements to improve health outcomes? Get our five tried and tested patient engagement best practices.